Adult assessment
Clinical assessment
To monitor ongoing, active disease, clinical assessment of weight, mobility, and pain should be conducted every year.1
Radiographic, renal, and biochemical monitoring can be used.
Radiographic
Renal
Biochemistry
Physical function & mobility
Regular assessment
Scheduled skeletal assessment of XLH patients is indicated. The frequency of review may vary depending on symptoms and surveillance of therapy.2
Bones
Lower-limb deformity
Height reduction, severity of leg deformity, and number of surgical corrections of leg deformities are indicators of skeletal disease severity.5
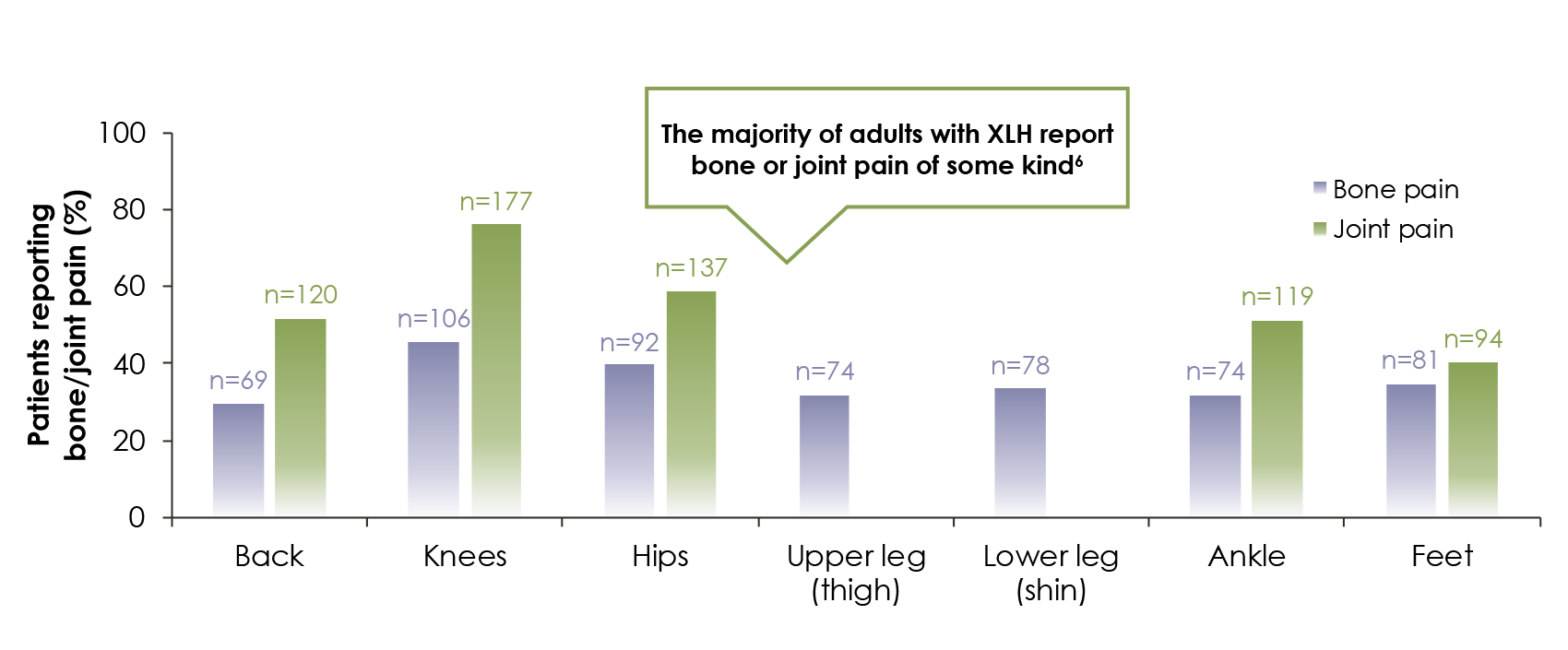
Osteoarticular symptoms
Pain, reduced physical function, and poor quality of life should trigger assessment of the origin of osteoarticular symptoms via skeletal survey and evaluation of biochemical parameters for evidence of osteomalacia.1
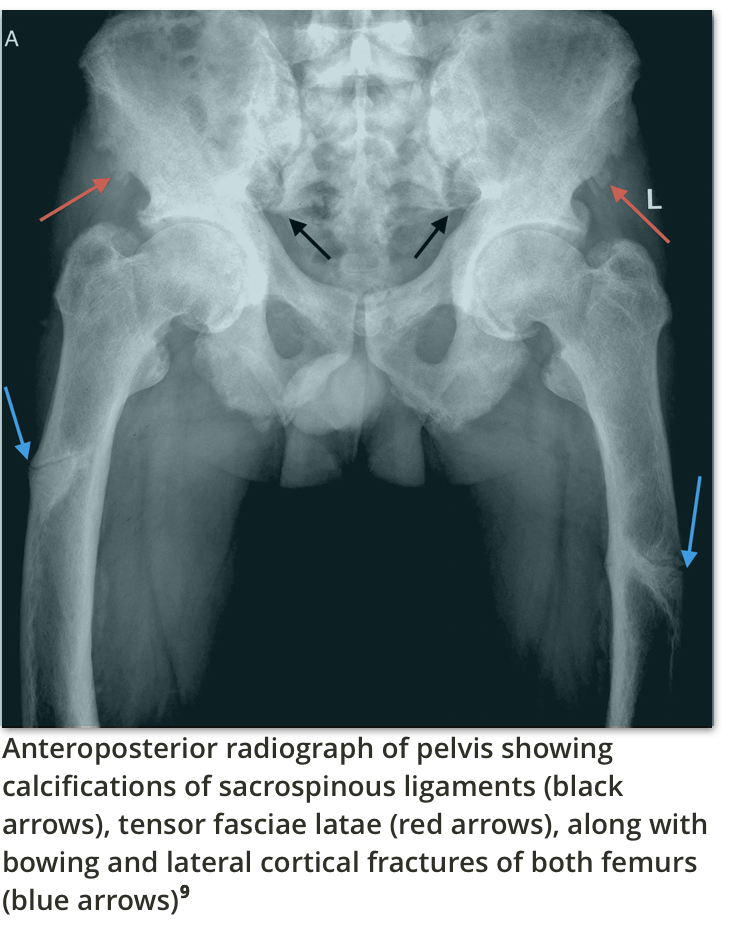
Fractures (including insufficiency fractures and Looser zones pseudofractures)6
The most common areas of insufficiency fractures are the femurs, feet, and tibiae/fibulae, followed by the hips, hands, and wrists.
Indications of insufficiency fractures might include:
- Insufficiency/Looser zones (Milkman lines)7
- Bone pain and focal tenderness3
- Nonunion
- Pseudoarthrosis8
Bone or joint pain6
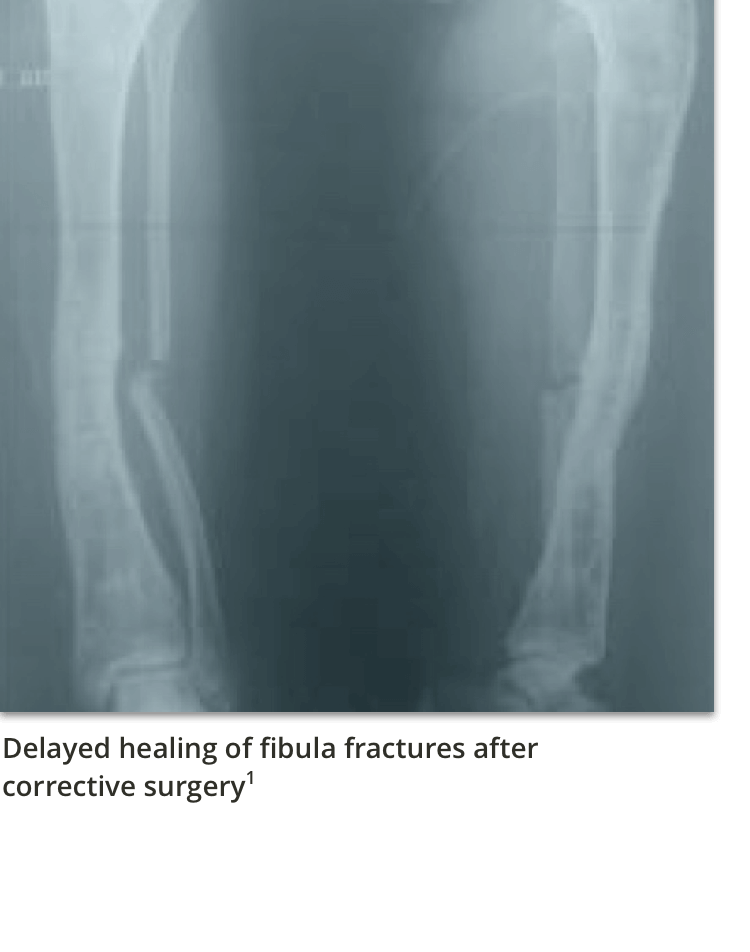
Surgical Interventions
Persistent lower-limb bowing and/or torsion resulting in misalignment of the lower extremity may require surgery. Patients may undergo surgical treatment to straighten the lower limbs (ie, osteotomy), or they may require hip or knee arthroplasty due to degenerative joint disease and enthesopathy.2
The aim of current treatment is to improve the symptoms, not to normalise serum phosphate levels.1
Joints and ligaments
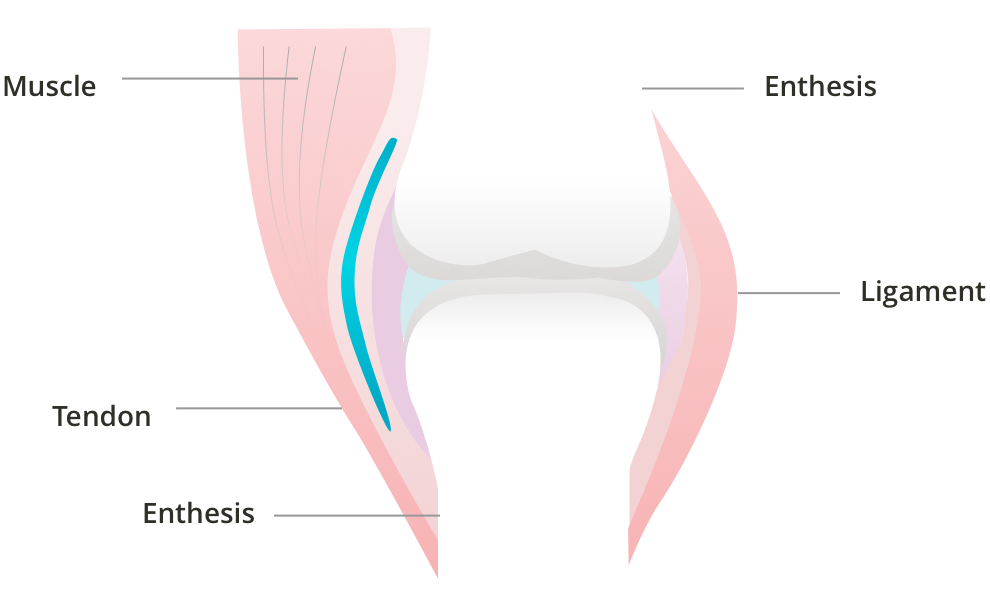
Enthesopathies are predominantly observed in those aged 40+.5
Enthesopathies are specialised attachments of tendon/ligament to bone resulting from inappropriate mineralisation.10
Dental
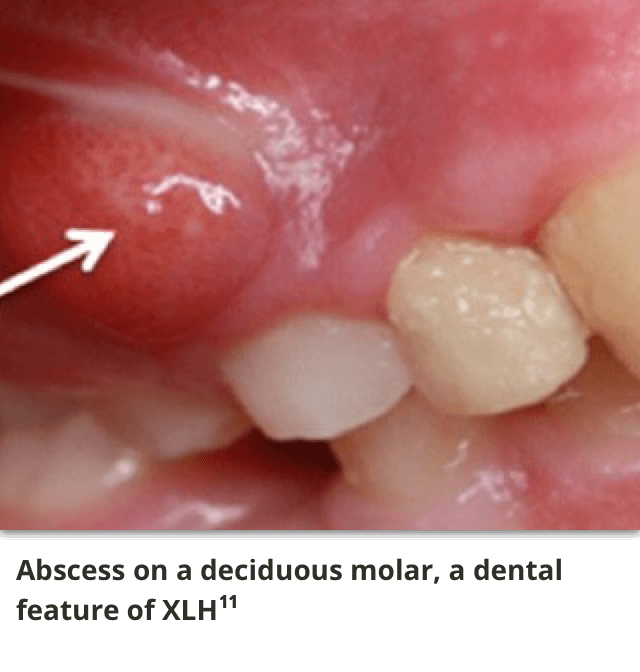
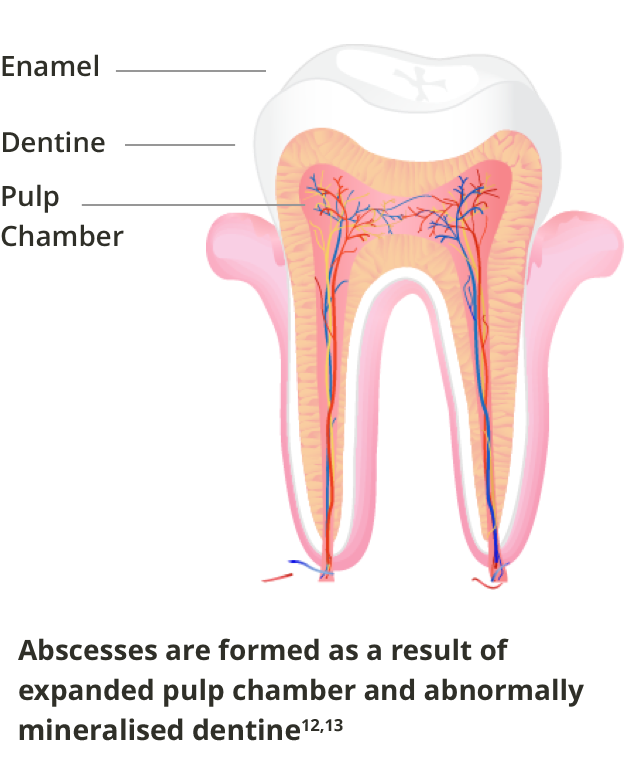
The dominant dental feature in XLH is the occurrence of spontaneous infection of the dental pulp tissue, resulting in tooth abscesses. In contrast with common endodontic infection, these abscesses develop in teeth without any signs of trauma or decay, affecting both the deciduous and permanent dentition.1
Adult patients with dental manifestations should be referred to a dental specialist with experience in XLH for a full clinical and radiographic examination.
Treatment options for dental abscesses in adulthood include1:
- Root canal cleaning
- Sealing the tooth surface with a dental resin to form a barrier to bacterial penetration
Prevention recommendations include1:
- Rigorous oral hygiene and preventive procedures
- Daily use of fluoride toothpaste adapted to age
- Regular fluoride varnish applications at the dental chair
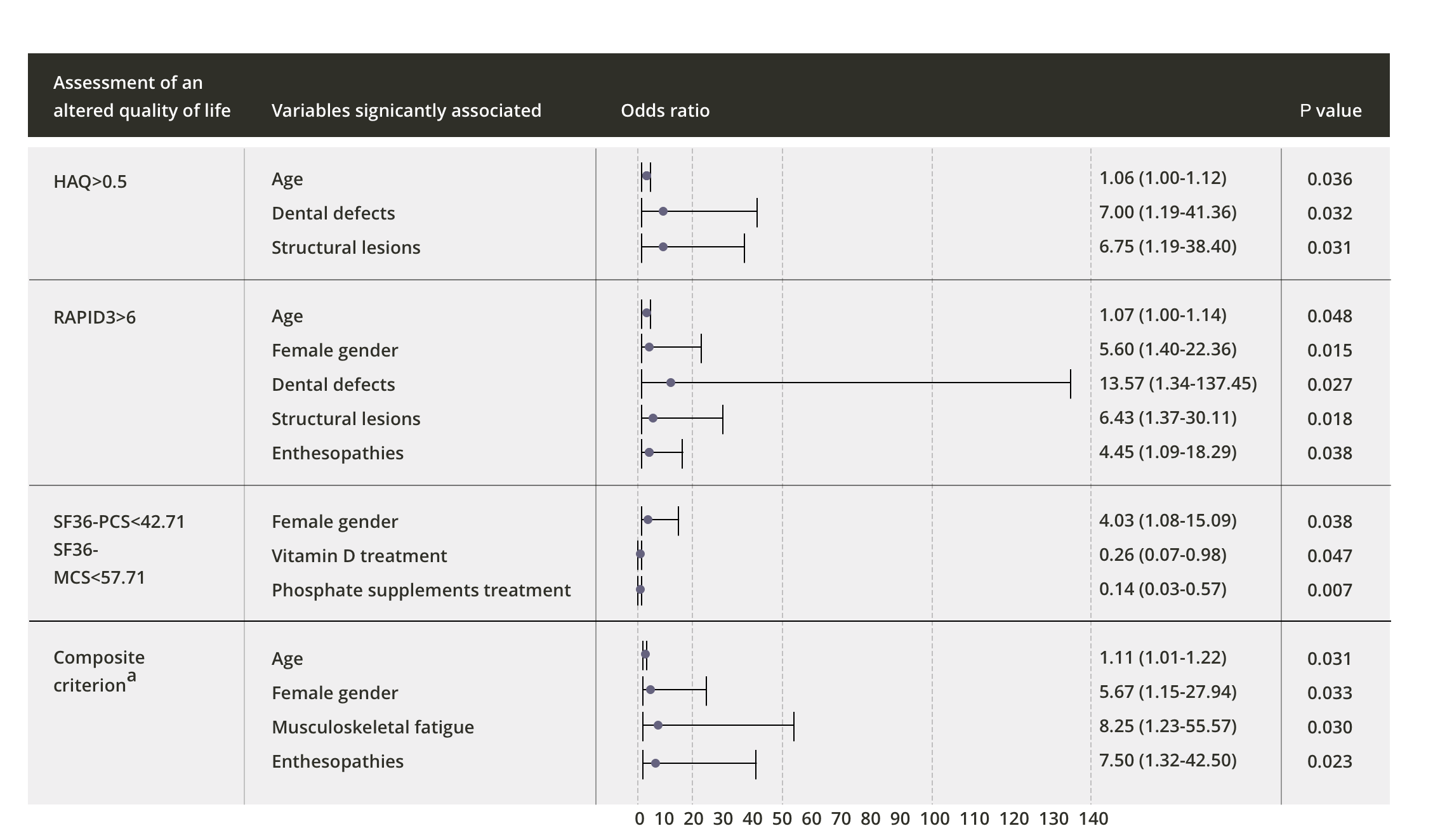
Quality of life in adults with XLH is affected most negatively by physical function, stiffness, and bodily pain. Impaired quality of life in adult patients may be an indicator of underlying skeletal disease.6
Radiographic imaging
Radiographic imaging can be used to assess the origin of osteoarticular symptoms such as bone/joint pain that lead to disability of physical function and poor quality of life.13
Walking ability
6-minute walk test (6MWT): The 6MWT is a practical, simple test that measures how far a patient can walk in 6 minutes on a flat, hard surface.14
Dental
Other quality of life tools
There are several quality-of-life tools that have been used to assess quality of life in adult XLH patients in studies and clinical trials. They include HAQ, SF-36, RAPID 3, and the composite criterion.15
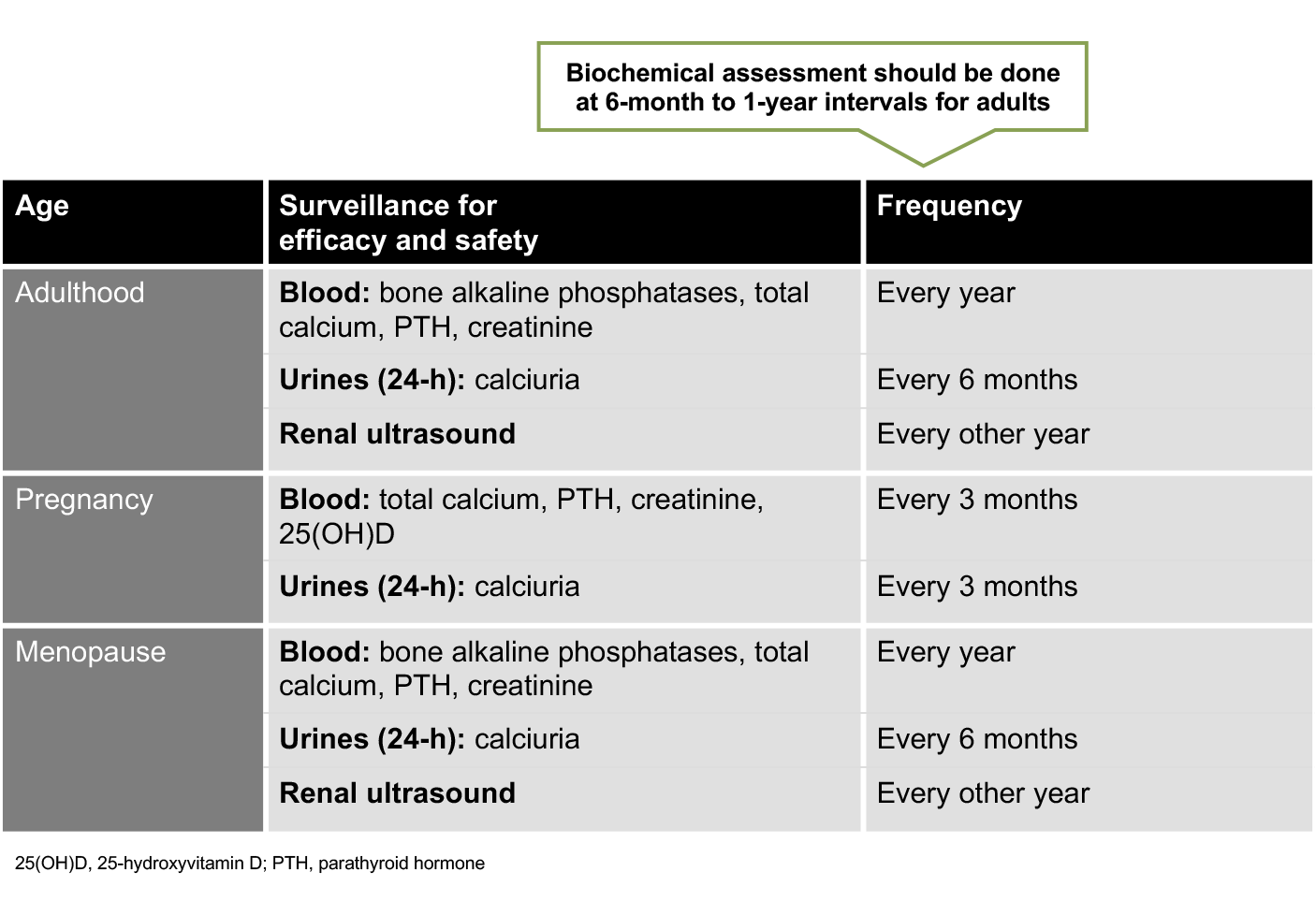
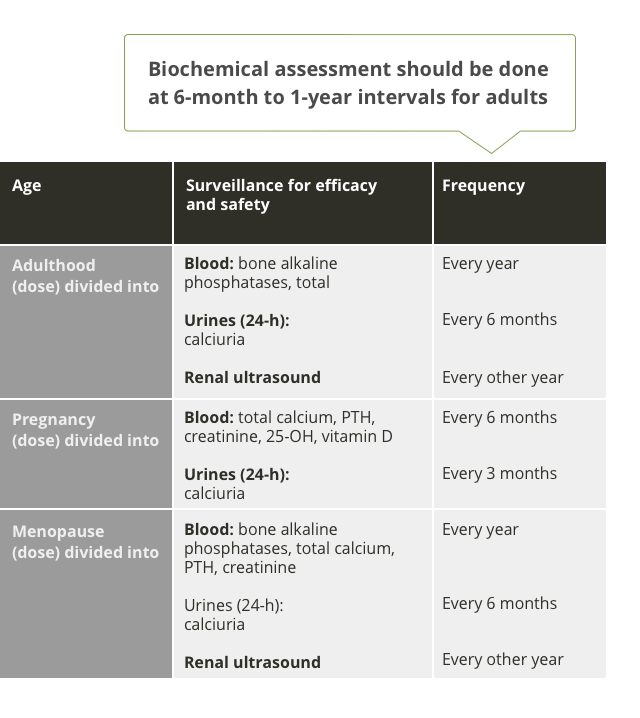
Biochemical monitoring
Regular monitoring is recommended to avoid hypercalcaemia, hypercalciuria, nephrocalcinosis, and hyperparathyroidism.1
Phosphate reabsorption
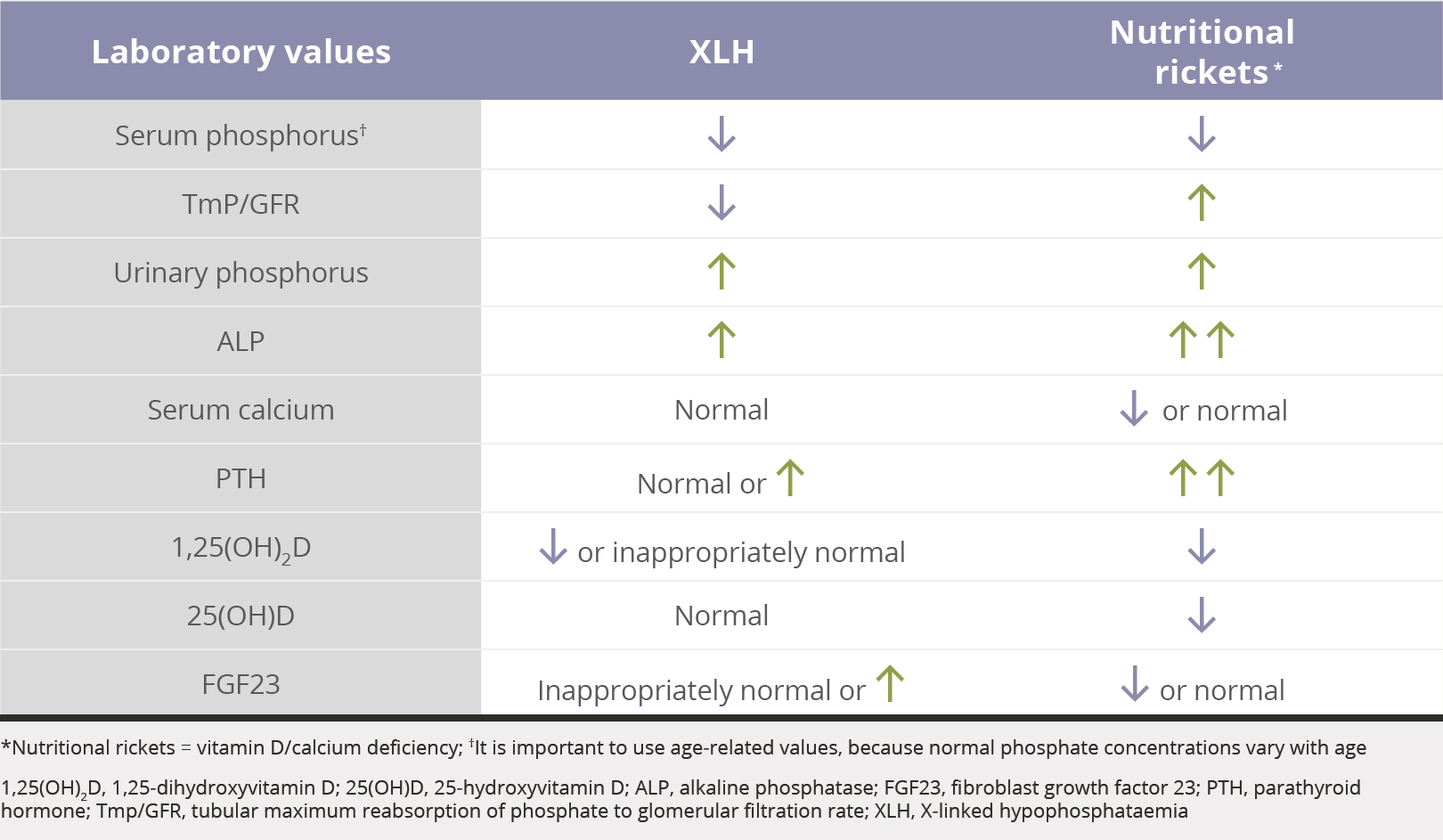
The TmP/GFR is the ratio of renal tubular maximum reabsorption of phosphate (TmP) to glomerular filtration rate (GFR)2,16-21